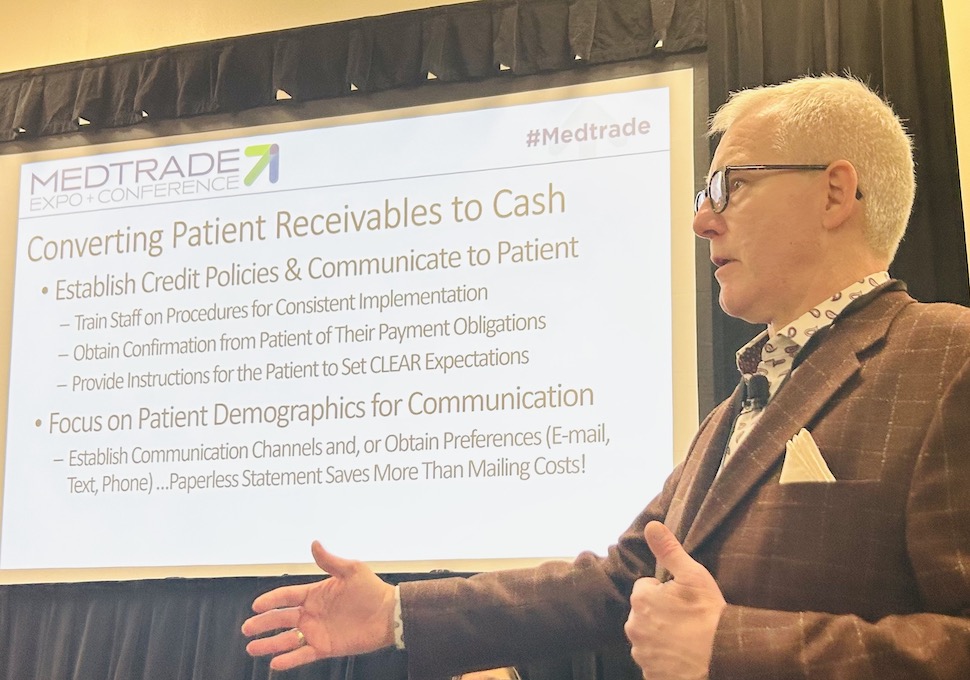
DALLAS – Last month’s Medtrade yielded a lot of practical advice and even a bit of inspiration. If you missed the panel discussion on retail / insurance operations, check out the extended excerpt from panelist Bruce Gehring who covered a basic question, namely; How can HME providers get paid with more consistency and efficiency?
 From Bruce Gehring, senior vice president, Business Development, Allegiance Group:
From Bruce Gehring, senior vice president, Business Development, Allegiance Group:
“We all need to get paid, but how do we do that? We need to start with the end in mind. We have to do a much better job of training staff. Those little differentiations allow you to get that cash payment.
“It comes down to policies and procedures. It’s missed so many times because people don’t take the time to really think through their product lines and make sure that they understand what the restrictions are [surrounding retail] and what the work-arounds are so that you can get paid.
“We don’t want to do the ‘claw back’, because then you have to reimburse Medicare for stuff that you did not qualify for. Make sure you have your account staff trained on those critical lines that follow under these variables.
“How do you connect with customers? It’s about getting them the information that’s available. You must have a procedure to follow up with patients and get that demographic information that you’re going to need so that you can follow up later—which is getting their cell phone and getting their e-mail. You will have that in the record so that you can communicate with them.
“And if we’re doing the rental; I don’t know how many times we’ve talked with providers who say; I get that first month’s rental up-front, but it’s going to be capped rental for 13 months. What about the subsequent months and getting the auto-pay set up so that when it does hit every month you’re getting paid? No exceptions.
“Make sure you have clear expectations with customers, because it’s so important. Make sure they understand their responsibilities. If they know, they will sign the authorization and know they’re going to be paying—but it has to be disclosed. You must have procedures and policies in place to follow up.
“We talk about auto-payments, but some of this goes back to educating referral sources. They have to understand what you need to be able to be reimbursed. Anytime you go to your doctor, you’re paying your copayment before you walk in to see the doctor. There’s no difference for us.
“How do you make it easy for your customers to pay you? There is the old fashioned way of filing the claim, determining the patient responsibility, billing the patient, and then hoping they’re going to pay you. That is the worst way to expect that you’re going to get full reimbursement. If you go that route, you’re leaving 40% to 50% of the cash on the table, and you can’t allow that, especially with reimbursements being cut more and more.
“That patient responsibility becomes the profit on a piece of equipment or the service that you’re providing. Make sure you’ve got processes in place to allow patients to connect with you. What do I mean by that? There’s simple things you can do, even in the billing process if you do send a bill—a QR code that takes a picture, for example, and opens up your payment portal.
 “If you’re doing E delivery, being able to have a link in the email that takes them to your payment portal, or text to pay, all those things. You’ve got to put the right tools in the tool locks, because some people say, ‘I’ll wait until I get the statement to pay’ but let’s let’s look at our demographic. Your patient age is coming up younger [even boomers] and they are used to e-mail and used to texts. You’ve got to be where your patients are, and be able to communicate with them in the manner they prefer.
“If you’re doing E delivery, being able to have a link in the email that takes them to your payment portal, or text to pay, all those things. You’ve got to put the right tools in the tool locks, because some people say, ‘I’ll wait until I get the statement to pay’ but let’s let’s look at our demographic. Your patient age is coming up younger [even boomers] and they are used to e-mail and used to texts. You’ve got to be where your patients are, and be able to communicate with them in the manner they prefer.
“When you get into setting up auto-pay and things like that, have some flexibility there. Make sure there are no barriers there for them to sit there and say, ‘I don’t want you just charging my credit card whenever.’ Make sure patients have the ability to set up when the credit card is going be charged, so they feel like they’re in control. And if you can do that, that’s huge, because now there is no excuse.
“If they get their social security check on the third week of the month, set up the charge on the 25th or whatever the appropriate date is so they can put it in their budget—and you know it’s going to hit on that date. If they are working, set it up on their payroll cycle.
“Make sure that you have that in your policies and procedures. Train your people on how to engage customers to get them set up on those auto-pays so you’ve got the guarantee [of payment]—because you’ve got to get paid. There’s no way around it.”

