WASHINGTON, D.C. – Late last year, CMS published the 2026 DMEPOS Fee-for-Service Fee Schedule. The fee schedule went into effect on Jan. 1, 2026 and includes the 2.0%-2.8% CPI-U adjustments announced in AAHomecare’s Dec. 22 alert.
The 2026 schedule includes the new intermittent catheter codes that will officially go into effect on January 1, 2026. Providers can download the 2026 fee schedule here. AAHomecare will be providing further analysis of the new rates after the new year.
New Intermittent Catheter Codes in Effect
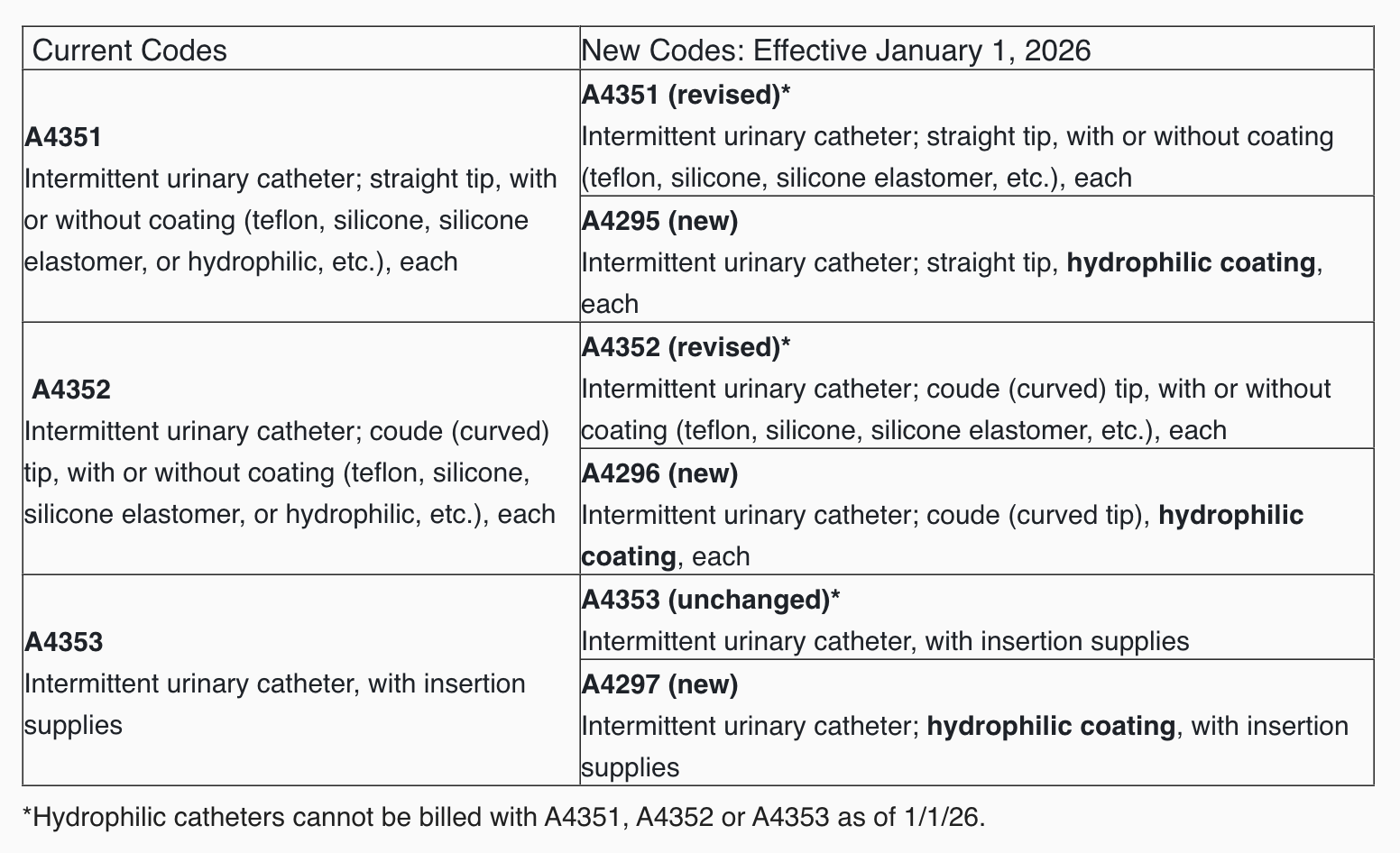
Starting in the new year, CMS will be revising two current intermittent catheter (IC) codes and is establishing new HCPCS codes for ICs with hydrophilic coating. HCPCS coding changes are in the chart below.
CMS’s Pricing Data Analysis and Coding (PDAC) contractor has also published the product classification list (PCL) crosswalk of the impacted codes. In the document, CMS notes that not all products qualified as ‘hydrophilic’ and were therefore not assigned to one of the new codes. Manufacturers may request for their product to be re-reviewed by submitting a Code Verification Review application to the PDAC.

