WASHINGTON, DC – On Nov. 1, CMS put out a request for comments to include certain ventilator classes (HCPCS codes E0465, E0466, and E0467) in the next round of the competitive bidding program, as well as adding several knee and back brace HCPCS codes to the CBP.
The downside of adding ventilators, which are highly specialized and service-intensive products, is clear to respiratory service providers who have first-hand knowledge of ventilators’ critical importance to patients with serious health issues.
“Ventilators are literally life support systems for the individuals who use them,” said Tom Vorhees, CEO of PromptCare, a respiratory and infusion therapy provider serving both adult and pediatric ventilator patients throughout the Mid-Atlantic and Northeast regions. “Including these products in the bidding program is guaranteed to reduce the number of companies with the experience and clinical expertise needed to serve this vulnerable patient cohort. If CMS’ decision to include ventilators in competitive bidding results in a lack of access to these critically important products, the impacts on Medicare and Medicaid beneficiaries and their caregivers will be devastating.”
“After years of decimating access to home medical equipment and supplies due to the unsustainable competitive bid program, CMS now wants to attack the technologies used by its most vulnerable beneficiaries,” adds Al Neumann, RCP, RRT, NPS, CPFT, vice president of Minnesota-based Corner Home Medical. “Respiratory companies need to make significant investments to train caregivers, stock backup equipment and supplies, and provide 24/7 therapists on call to make sure patients can avoid hospital visits and other clinical interventions. I’d like CMS to tell us what part of those services they would like us to cut back on when bidding drives down reimbursement rates even further.”
“Awarding contracts for life support equipment to lowest bidders is going to have grave consequences for patients, families, and other medical professionals who support this community,” concludes Neumann. “It’s bad policy, and it’s going to cause a lot of suffering for people who depend on ventilators”
Make Sure CMS Gets the Message!
We need to send a clear and compelling message that adding ventilators to the bidding program is clinically unsound and will severely impact vulnerable patients. Please share your concerns with CMS by Monday, December 17 via [email protected].
We have developed a brief messaging document to help you formulate your comments and make the case for keeping ventilators out of the bidding program. It is important to personalize your comments by explaining the types of ventilator patients you serve and the services you provide them, and how they will be impacted if CMS includes ventilators in the competitive bidding program.
Our messaging document also provides language asking CMS to provide more specific coverage criteria for ventilators instead of adding these products to the bidding program.
Please share this message with any patients, clinicians, hospitals, caregivers, or respiratory patient groups and encourage them to share comments with CMS on the need to maintain patient access to ventilators by keeping them out of the bidding program. Just like the HME community, these individuals should be “engaged and enraged” to make sure these critically important products and services remain fully available.
AAHomecare has consistently advocated for keeping ventilators out of the bidding program, including recent comments to MedPAC (see page 4) on the issue. We are also working with respiratory therapy clinician groups, as well as patient advocacy groups with constituencies who depend on these products, to echo our concerns in their comments to CMS.
AAHomecare will also share comments when they are completed.
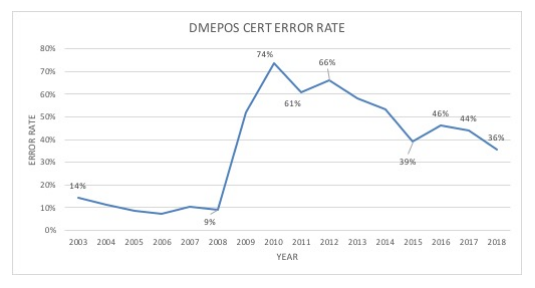
DMEPOS Improper Payment Rate Continues to Decline
WASHINGTON, DC – CMS has announced that the DMEPOS improper payment rate decreased from 46.2% in 2016 to 35.5% in 2018, representing a $1.14 billion decrease in improper payments. Overall, the Medicare fee-for-service improper payment rate dropped from 9.5% in 2017 to 8.1% in 2018.
In June of this year, AAHomecare and several members of our Regulatory Council met with CMS’s Comprehensive Error Rate Testing (CERT) team in Baltimore to get further clarification on the Agency’s 2017 improper payment data and to explore ways to continue to improve error rates.
You can see more in CMS’ blog post and related fact sheet on the issue. We will provide additional analysis when CMS releases a new Improper Payments Report or related data.
Turnover on Capitol Hill Presents Challenge and Opportunity for HME Advocacy
With 100 new members of Congress to take office on January 3rd, HME advocates will have both the challenge and the opportunity to educate these incoming lawmakers on the need for sustainable reimbursement and sensible regulatory policy for our industry.
 If you worked on a campaign or have any connections to the new members (or if you’re just a constituent of theirs) joining the 116th Congress, please make sure to reach out to them to offer congratulations and let them know you’ll be following up to discuss HME policy after they take office. Please contact Gordon Barnes at [email protected] to let us know of any direct connections you have to the new legislators, as well. You can see more about the incoming members of Congress here.
If you worked on a campaign or have any connections to the new members (or if you’re just a constituent of theirs) joining the 116th Congress, please make sure to reach out to them to offer congratulations and let them know you’ll be following up to discuss HME policy after they take office. Please contact Gordon Barnes at [email protected] to let us know of any direct connections you have to the new legislators, as well. You can see more about the incoming members of Congress here.
The HME community made great strides in raising the profile of HME policy priorities in the 115th Congress, which ultimately translated into strong Congressional support on sign-on letters and direct outreach to CMS on the HME-related IFR and the ESRD/DMEPOS Final Rule. With so much turnover in the wake of the 2018 mid-term elections, we need to redouble our engagement on Capitol Hill in 2019. We’ll have more on renewing our advocacy work on Capitol Hill in upcoming editions of Wednesday in Washington.

