 WASHINGTON, DC – Telehealth is the wave of the future. In many instances, a telehealth encounter with a physician is more efficient and effective than a face-to-face encounter between the physician and patient. Unfortunately, telehealth encounters and Medicare coverage for DME do not yet go hand- in-hand.
WASHINGTON, DC – Telehealth is the wave of the future. In many instances, a telehealth encounter with a physician is more efficient and effective than a face-to-face encounter between the physician and patient. Unfortunately, telehealth encounters and Medicare coverage for DME do not yet go hand- in-hand.
The industry is witnessing an increasing number of physician orders for DME that arise out of a telehealth physician/patient encounter. However, we are also witnessing Medicare denying reimbursement for claims for DME arising out of telehealth encounters.
A case in point is a payment suspension letter that a DME supplier recently received from a ZPIC/PSC. The letter says, in part:
The purpose of this letter is to notify you of our determination to suspend Medicare payments to ________, pursuant to 42 C.F.R. §405.371(a)(1). The decision to suspend your Medicare payments was made by the Centers for Medicare & Medicaid Services (CMS) and is based on reliable information that an overpayment exists and that payments to be made may not be correct.
The suspension of your Medicare payments took effect on _____, 2016. This suspension may last for 180 days from the effective date of the suspension and may be extended under certain circumstances. See 42 C.F.R. §405.372(d). Prior notice of this suspension is not being provided because giving prior notice would place additional Medicare funds at risk and hinder our ability to recover any determined overpayment. See 42 C.F.R. §405.372(a)(3).
As noted above, the suspension of your Medicare payments is based on reliable information that an overpayment exists, and that payments to be made may not be correct. See 42 C.F.R. §405.371(a)(1). Specifically, the suspension of your Medicare payments is based on, but not limited to a review of the documentation you submitted to [Name of ZPIC/PSC] for a prepayment audit conducted on claims you submitted to Medicare in which supporting documentation was requested from your facility. Our review found that LCD coverage criteria were not met as required examination of joint laxity was not documented or the medical records documented a joint laxity test that could not have occurred via telehealth visit. The review resulted in a __% denial (__/__ claims).
Examples of such billings include, but are not limited to, the following:
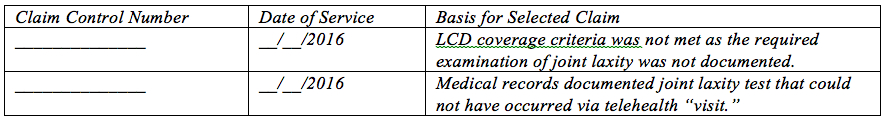
This list is not exhaustive or complete in any sense, as our investigation into this matter is continuing. The information is provided by way of example, in order to furnish you with adequate notice of the basis for the payment suspension noticed herein.
[Name of ZPIC/PSC] has initiated a process to review your Medicare claims and supporting documentation prior to payment. The purpose of implementing this prepayment process is to ensure that all payments made by the Medicare program are appropriate and consistent with Medicare policy. The prepayment process is often applied to safeguard Medicare from unnecessary utilization of services furnished by providers, and to ensure that no Medicare payments are made for items and services that “are not reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of a malformed body member [.]” See Social Security Act 1862(a)(1)(A). Notification is hereby given that you are expected to comply with the prepayment process for claims for all services and all dates of services.
This letter addresses claims for knee braces. These claims arise from telehealth encounters. Specifically, the ordering physician only had a telephone conference with the patient. In denying some of the claims, the ZPIC/PSC stated that there was no documentation of an examination of joint laxity. In denying other claims, the ZPIC/PSC stated that while there is documentation of a joint laxity examination, such an examination could not have occurred with a telehealth encounter.
According to CMS, Medicare beneficiaries are eligible for telehealth services only if they are presented from an originating site located in:
• A rural Health Professional Shortage Area (HPSA) located either outside of a Metropolitan Statistical Area (MSA) or in a rural tract; or
• A county outside of a MSA.
CMS defines originating sites as:
• Offices of physicians or practitioners;
• Hospitals;
• Critical Access Hospitals (CAHs);
• Rural Health Clinics;
• Federally Qualified Health Centers;
• Hospital-based or CAH-based Renal Dialysis Centers (including satellites);
• Skilled Nursing Facilities (SNFs); and
• Community Mental Health Centers (CMHCs).
Medicare further states that as a condition of payment, there must be an interactive audio and video telecommunications system that permits real-time communication between the practitioner, at the distant site, and the beneficiary, at the originating site.
Information from CMS suggests that even if a telehealth encounter complies with state telehealth laws, and even if a claim is not submitted to Medicare for the telehealth visit, Medicare will deny the claim for DME if the physician order arises from a telehealth encounter that does not meet the requirements set out above.
Denise Leard will be presenting the following webinar:
AAHOMECARE’S EDUCATIONAL WEBINAR
Waiver or Reduction of Medicare and Commercial Co-Payments: What You Can and Cannot Do
Presented by: Denise M. Leard, Esq., Brown & Fortunato, P.C.
Tuesday, October 4, 2016
2:30-4:00 p.m. EASTERN TIME
DME suppliers have an obligation to take reasonable steps to collect co-payments from Medicare beneficiaries. Of course, this is easy to do when the beneficiary has supplemental insurance. This is not quite so easy when the beneficiary does not have supplemental insurance. From the viewpoint of the OIG, it is important for the beneficiary to pay something. This causes the beneficiary to have “equity” in the process thereby making the beneficiary a wiser consumer of health care products and services. When a DME supplier routinely waives co-payments … and particularly when the supplier advertises that it waives co-payments, then the OIG considers this to be a kickback, inducement, and a false claim. According to the OIG, the supplier can only waive a co-payment when the supplier has made a patient-specific decision to waive … and that decision is based on the financial condition of the beneficiary. Interestingly, contracts with commercial insurers and state statutes impose substantially the same requirements on DME suppliers that bill commercial insurers. This program will discuss the requirements imposed upon DME suppliers to attempt to collect co-payments from Medicare beneficiaries and commercial patients, and the steps that the supplier should take before waiving a co-payment.
Register for Waiver or Reduction of Medicare and Commercial Co-Payments: What You Can and Cannot Do on Tuesday, October 4, 2016, 2:30-4:00 pm ET, with Denise M. Leard, Esq., of Brown & Fortunato, PC.
Please contact Ika Sukh at ikas@aahomecare.org if you experience any difficulties registering.
FEES
Member: $99.00
Non-Member: $129.00
Jeffrey S. Baird, JD, is chairman of the Health Care Group at Brown & Fortunato, PC, a law firm based in Amarillo, Tex. He represents pharmacies, infusion companies, HME companies and other health care providers throughout the United States. Mr. Baird is Board Certified in Health Law by the Texas Board of Legal Specialization, and can be reached at (806) 345-6320 or jbaird@bf-law.com.

